Disclaimer: People of any gender can experience painful sex. This article is referring specifically to pain with vaginal penetration, but stay tuned for future posts that explore other types of sexual pain.
How common is it to have painful sex?
According to the American College of Obstetricians and Gynecologists (ACOG), nearly 75% of women will experience pain during sex at some point in their lives. This means that many of the women in your life have likely experienced it, even if they aren’t talking about it.
What causes pain with penetration?
There are many potential causes for pain with penetration including pelvic floor dysfunction, vulvar skin disorders, vaginal atrophy, endometriosis, pelvic inflammatory disease, pelvic organ prolapse... the list goes on! One of the most common reasons is that the muscles of the pelvic floor are overactive – this can mean that they contract when they should be relaxing or that they remain in a chronically tightened position.
The pelvic floor acts as a sling to support our organs as well as assist with bowel, bladder, and sexual function. When these muscles are overactive, this can lead to dyspareunia (pain with penetrative sex) as well as other urinary and/or bowel symptoms.
Where is the pain?
The source of vaginal pain during penetration can be superficial, deep, or a mixture of both. If pain has lasted longer than three months, the brain and nervous system could be playing a role.
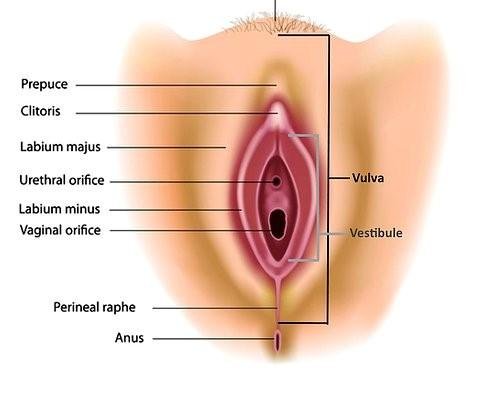
Superficial: This refers to pain at the entrance of the vagina, also known as the introitus. Pain at the vestibule (just inside the inner lips of the vulva) can be caused by hypersensitive nerve endings in this area or may be hormone-related.
Sometimes, pain at the entrance to the vagina can be due to a condition called vaginismus, which is when involuntary muscle spasms of the pelvic floor close the vaginal opening. Some women describe this feeling as “hitting a wall” when they try to have sex or insert a tampon.
Deep: This pain is often felt in the cervix or abdomen and can be worsened with certain sexual positions. This can be due to conditions that affect the pelvis, such as endometriosis or pelvic inflammatory disease.
Brain and nervous system: If the pain has lasted more than three months, this can cause nerves to become more sensitive to stimuli. Anxiety, stress, and fear can all play a role in how the brain interprets signals that relate to pain response.
What can help?
The first step is to talk to a medical provider about your symptoms. Your ob/gyn can diagnose your condition and provide you with treatment options, including referral to a pelvic health physical therapist.
What is pelvic health physical therapy?
Pelvic health PTs have specialized training in assessing the pelvic floor, as well as other muscles, nerves, and joints surrounding the pelvis. Treatment is highly individualized to ensure that patients feel safe and comfortable during their sessions.
You might be wondering how PTs assess the pelvic floor, and there are a variety of ways. For patients who prefer to stay fully clothed, the muscles can be assessed using a hand placed underneath the sit bone. If patients are open to an internal exam, a PT can insert a single finger vaginally to assess the pelvic floor. This is fully at the patient’s discretion and is a gradual process, especially for those in pain.
Treatment can include:
Strategies for activating and relaxing the pelvic floor
Trigger point therapy for tight muscles
Recommendations for lubricants, topical ointments, and devices to decrease pain and improve function
Education on ways to stretch and release the pelvic floor, including use of a finger or dilators
Other important factors
Mental health: Painful sex is more than just a physical condition. There are so many emotions wrapped up in a person’s sexual experience, and these can have an impact on the brain’s pain response. It’s completely normal to experience feelings of anxiety, shame, and/or depression when faced with this condition. In conjunction with physical therapy, it may be helpful to talk to a mental health provider to discuss unhealthy beliefs and fears, such as “will it always be this painful?” “what’s wrong with me?” or “what will my partner think?”
Communication with your partner: This is key! Often, women place blame on themselves when they are experiencing painful sex, but it takes two to tango. Sharing your feelings with a partner might feel vulnerable, but it opens the door for ways to improve the experience for both of you.
Talking about sex doesn’t always have to be serious or scary, though. Simply telling a partner what feels good and playfully experimenting can be both fun and beneficial for pain. It’s been scientifically proven that arousal can decrease the pain response, so make sure you’re finding ways to enjoy the experience.
And remember, sex can be any activity that leads to arousal and does not need to involve penetration at all. If you are being pressured to engage in sexual activities that don’t feel right for you, it may be helpful to find a mediator, such as a sex therapist, to aid in discussing these issues with your partner.
Devices that can help! However, with ads making all kinds of crazy claims about how to improve your sex life, it can be overwhelming to try to find a product that is actually effective and worth the money. We give you a few options in the next section.
Helpful devices for painful sex
Dilators - used for progressive stretching, come in a variety of sizes, typically made out of silicone or plastic.
Vibrators - can be used in so many different ways, internally or externally to stimulate arousal and promote “vibratory analgesia,” which decreases pain.
Buffer rings - rings placed around a partner’s shaft to decrease the depth of penetration, especially helpful for those who suffer from deep vaginal pain.
Lotions and lubes: Lubricant can be helpful to decrease pain during sex and make the experience more pleasurable. Avoid lubes with lots of chemical additives or fragrance, such as essential oils, glycerin, or artificial flavor. Try to choose one that reflects the pH of a healthy vagina (around 3.8-4.5) to prevent increased risk of bacterial infection.
Topical Lidocaine is a numbing cream that can be used at the vaginal opening or vestibule to reduce pain. Some people worry that this will affect arousal, but when used in a small, localized area, it is unlikely to impact sexual sensation. It is now available over the counter at a 5% concentration.
Vaginal estrogen or testosterone cream: If a hormonal imbalance is causing your pain, a medical provider can prescribe topical estrogen or testosterone. Topical estrogen is often prescribed for vaginal atrophy, which can occur during or after menopause. Both estrogen and testosterone have been found effective in the treatment of vestibulodynia (pain at the vestibule).